All topics are updated as new evidence becomes available and our peer review process is complete.
INTRODUCTION — Gallstones are common, particularly in Western populations ( table 1 ). In the United States, gallstones are seen in approximately 6 percent of men and 9 percent of women. Most individuals with gallstones are asymptomatic throughout their lives. When the stones start causing symptoms, the condition is referred to as gallstone disease. Uncomplicated gallstone disease refers to stones in the gallbladder that are associated with biliary colic in the absence of complications, such as acute cholecystitis, cholangitis, or gallstone pancreatitis.
Determining whether a patient’s upper digestive symptoms are the result of gallstones detected on imaging can be challenging. While both gallstones and upper digestive symptoms are common in the general population, they are not always related. Differentiating patients with uncomplicated gallstone disease from those with other disorders and an incidental finding of gallstones is important, since cholecystectomy is often curative in those with symptomatic gallstones, but it exposes those with incidental gallstones to unnecessary risk, delays appropriate treatment for the actual cause of symptoms, and incurs unnecessary expense.
This topic will review uncomplicated gallstone disease. The epidemiology of and risk factors for gallstones, the approach to patients with an incidental finding of gallstones, gallstone disease in pregnant women, and the complications of gallstone disease are discussed separately. (See “Epidemiology of and risk factors for gallstones” and “Approach to the patient with incidental gallstones” and “Gallstone disease in pregnant women” and “Pathogenesis, clinical features, and diagnosis of acute cholecystitis” and “Etiology of acute pancreatitis”, section on ‘Gallstones’ and “Acute cholangitis” and “Approach to the patient with suspected choledocholithiasis” .)
CATEGORIZATION OF PATIENTS — When considering gallstone disease, we have found it helpful to categorize patients into the following clinical groups:
- Category 1: Gallstones on imaging studies but without symptoms (incidental gallstones)
- Category 2: Typical biliary symptoms and gallstones on imaging studies with no evidence of complications (uncomplicated gallstone disease)
- Category 3: Atypical symptoms and gallstones on imaging studies
- Category 4: Typical biliary symptoms but without gallstones on ultrasound
As will be discussed below, the approach to patients in categories 1 and 2 is generally straightforward. Patients in category 1 should generally be left alone, while those in category 2 should undergo treatment aimed at eliminating the gallstones. By contrast, optimal approaches to patients who fall into the last two categories (3 and 4) are less clear. Management of such patients should be individualized and depends largely upon the likelihood (based upon clinical features and diagnostic testing) that the patient’s symptoms are related to the gallstones. (See ‘Management’ below.)
NATURAL HISTORY — The majority of patients with gallstones are asymptomatic. Of those with incidental (asymptomatic) gallstones, approximately 20 percent will develop symptoms over 15 years of follow-up, but their initial symptoms are typically not severe [ 1 ]. (See “Approach to the patient with incidental gallstones”, section on ‘Natural history of asymptomatic gallstones’ .)
Among patients with symptoms the natural history is variable, ranging from symptom resolution to the development of severe complications. This was demonstrated in a study that included 94 patients with mild symptoms and 119 patients with severe symptoms [ 2 ]. The patients were followed for a mean of 8.7 years. At the end of follow-up, 58 percent of the patients with mild symptoms were asymptomatic, 17 percent had mild symptoms, and 25 percent had severe symptoms. On the other hand, 52 percent of those with severe symptoms were asymptomatic, 17 percent had mild symptoms, and 31 percent had severe symptoms.
Complications that may develop in patients with gallstones include acute cholecystitis, choledocholithiasis with or without acute cholangitis, and gallstone pancreatitis. Acute cholecystitis is the most common complication. In a systematic review, it was seen in 6 to 11 percent of patients with symptomatic gallstones over a median followup of 7 to 11 years [ 3 ]. Rare complications include gallbladder cancer, gallstone ileus, and Mirizzi syndrome.
Patients with asymptomatic gallstones appear to have a slightly lower risk of complications than those with symptomatic gallstones. This was demonstrated in a study that followed 123 patients with asymptomatic gallstones and 298 patients with mild symptoms due to gallstones for up to 25 years [ 4 ]. It found that the cumulative probability of developing severe complications was lower among patients with asymptomatic gallstones compared with those with mild symptoms after 5, 10, 15, and 20 years of follow-up (4 versus 5 percent, 5 versus 12 percent, 10 versus 15 percent, and 16 versus 18 percent, respectively; p = 0.03).
CLINICAL FEATURES — Patients with uncomplicated gallstone disease typically present with biliary colic, normal physical examination findings, and normal laboratory test results. Patients often report associated diaphoresis, nausea, and vomiting.
While patients may present with atypical symptoms, such as chest pain or nonspecific abdominal discomfort, the absence of biliary colic should prompt an investigation for alternative diagnoses. On the other hand, biliary colic that is associated with fevers, jaundice, or abnormal blood tests (leukocytosis, liver tests, pancreas tests) suggests the development of a complication of gallstone disease. (See ‘Differential diagnosis’ below.)
Biliary colic — Despite the name, the pain of biliary colic is usually constant and not colicky. The classic description is of an intense, dull discomfort located in the right upper quadrant, epigastrium, or (less often) substernal area that may radiate to the back (particularly the right shoulder blade) [ 5,6 ]. The pain is often associated with diaphoresis, nausea, and vomiting. It is not exacerbated by movement and is not relieved by squatting, bowel movements, or passage of flatus [ 7 ].
Biliary colic is usually caused by the gallbladder contracting in response to hormonal or neural stimulation, forcing a stone (or possibly sludge) against the gallbladder outlet or cystic duct opening, leading to increased intra-gallbladder pressure. This increase in pressure then results in pain. Eating a fatty meal is a common trigger for gallbladder contraction, and many patients report postprandial pain. However, an association with meals is not universal, and in a significant proportion of patients the pain is nocturnal [ 8,9 ].
The pain typically lasts at least 30 minutes, plateauing within an hour. As the gallbladder relaxes, the stones often fall back from the cystic duct and the pain slowly subsides, with an entire attack usually lasting less than six hours [ 5 ]. In many patients, the pain is not severe, which is why patients often have had several attacks before seeking medical attention. The frequency of recurrent attacks is variable, ranging from hours to years, though most patients do not have symptoms on a daily basis [ 7 ]. Typically, the pain has a characteristic pattern and timing for an individual patient.
Atypical symptoms — Numerous symptoms other than biliary colic have been reported in patients with gallstones, but their predictive value for the presence of gallstone disease is poor. In many cases they may coexist with biliary colic but may or may not be related to the gallstones [ 10-12 ]. Atypical symptoms seen in patients with gallstones include:
- Chest pain
- Nonspecific abdominal pain
- Belching
- Fullness after meals/early satiety
- Fluid regurgitation
- Abdominal distension/bloating
- Epigastric or retrosternal burning
- Nausea or vomiting without biliary colic
Whether atypical symptoms are due to the gallstones or due to a coexistent problem can be difficult to determine. Patients with atypical symptoms without associated biliary colic should be evaluated for alternative diagnoses, even if gallstones are demonstrated on imaging. (See ‘Differential diagnosis’ below.)
Physical examination — Patients with biliary colic due to uncomplicated gallstone disease are usually not ill appearing and do not have fever or tachycardia. The pain is often not severe enough to bring the patient to the emergency department. If a patient does present during a pain episode, the abdominal examination is generally benign. Biliary colic is visceral pain and there are no peritoneal signs because the gallbladder is not inflamed. However, voluntary guarding may be encountered depending upon the severity of the pain.
Laboratory studies — Laboratory studies should be normal in patients with uncomplicated gallstone disease, both during asymptomatic periods and during attacks of pain. Abnormal blood tests (leukocytosis, elevated liver or pancreas tests) suggest the development of a complication of gallstone disease, such as cholecystitis, cholangitis, or pancreatitis. (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis” and “Acute cholangitis”and “Clinical manifestations and diagnosis of acute pancreatitis” .)
Imaging studies — Most patients with uncomplicated gallstone disease will have gallstones demonstrated on transabdominal ultrasound. Other imaging studies, such as plain abdominal x-rays or computed tomography (CT) scanning of the abdomen are less sensitive than ultrasound, though patients may have had the tests as part of the general evaluation of their abdominal pain. (See ‘Transabdominal ultrasound’ below.)
Plain abdominal x-rays rarely reveal gallstones because only about 10 percent of gallstones contain enough calcium to make them sufficiently radio-opaque to be visible on a plain radiograph ( image 1 ). The sensitivity of CT scan for gallstones has been reported to be 55 to 80 percent. Gallstones may be missed on CT because many stones are isodense with bile [ 13,14 ].
DIAGNOSIS — The diagnosis of uncomplicated gallstone disease should be suspected in a patient with biliary colic, a normal physical examination, and normal laboratory tests (complete blood count, aminotransferases, bilirubin, alkaline phosphatase, amylase, and lipase). Such patients should undergo an imaging study to determine if there are gallbladder stones or sludge. Typically, the evaluation begins with a transabdominal ultrasound since it is the most sensitive modality for detecting gallbladder stones. If the transabdominal ultrasound is negative in a patient with biliary colic, additional studies that may help with the diagnosis include endoscopic ultrasound (EUS) and bile microscopy.
Transabdominal ultrasound — Transabdominal ultrasound is generally considered to be the most useful test to detect the presence of gallstones since it is non-invasive, readily available, relatively inexpensive, and does not subject the patient to ionizing radiation. The examination should be conducted with the patient having fasted for at least eight hours, because stones are best seen when surrounded by bile in a distended gallbladder.
Characteristics of stones on ultrasound — Patients with uncomplicated gallstone disease may have ultrasound findings of gallstones, gravel, or sludge. Distinguishing among these three entities is generally not clinically important because they are managed identically. (See ‘Management’ below.)
On ultrasound, gallstones appear as echogenic foci that cast an acoustic shadow ( image 2 ) and seek gravitational dependency [ 15,16 ]. Gravel is the appearance of multiple small stones that are echogenic and cast shadows. Sludge is echogenic in appearance but does not cast an acoustic shadow. It is also more viscous and does not move to the dependent portion of the gallbladder as rapidly as gravel [ 17,18 ].
The sludge seen on ultrasound represents microlithiasis (lithogenic bile that contains cholesterol monohydrate crystals, bilirubin granules, and a mucus glycoprotein gel) [ 19,20 ]. Microlithiasis can produce biliary colic and lead to complications such as acute cholangitis and acute pancreatitis [ 21-25 ]. It may also progress to macroscopic gallstones [ 26,27 ].
False negative results may be obtained if the gallbladder is completely filled with stones or if it is contracted around many stones. In such cases, the findings may be confused with gas in a partially collapsed duodenal bulb, emphysematous cholecystitis, porcelain gallbladder, or a calcified hepatic artery aneurysm. False positive results may be seen if gallbladder polyps are present, since they produce sonographic images similar to those seen with gallstones, though they do not cast an acoustic shadow ( image 2 ). The ultrasonographer performing the procedure regularly uses specific maneuvers and techniques to identify and distinguish gallstones from some of these other entities. As a result, ultrasonography is highly operator-dependent. (See”Gallbladder polyps and cholesterolosis” .)
Test characteristics — Multiple studies have evaluated the ability of transabdominal ultrasound to detect gallstones, though it is important to recognize that precise estimates of sensitivity and specificity are difficult to determine since surgical confirmation of a negative sonogram is unlikely.
A systematic review estimated that the sensitivity was 84 percent (95% confidence interval [CI] 76 to 99%) and specificity was 99 percent (95% CI 97 to 100%) [ 28 ]. Rarely, advanced scarring and contraction of the gallbladder around gallstones leads to nonvisualization of the gallbladder lumen, which has a specificity of 96 percent, but it should also raise the possibility of gallbladder cancer.
When compared with other cross-sectional imaging modalities and cholecystography, ultrasound has the highest sensitivity [ 29,30 ]. Modern sonographic equipment is able to detect stones as small as 1.5 to 2 mm in diameter [ 29 ]. Smaller stones may be missed, and the sensitivity falls to 50 to 60 percent for stones less than 3 mm in diameter [ 31-33 ].
The accuracy of transabdominal ultrasonography is operator dependent. The entire gallbladder must be examined axially and sagittally. Every effort should be made to examine the outlet of the gallbladder (Hartmann’s pouch), where gallstones may be difficult to detect. The gallbladder neck must be traced all the way into the porta hepatis to exclude stones in this region. If an out-pouching from the gallbladder (Phrygian cap) is present, the redundant portion of the fundus must not be overlooked.
Even with an experienced operator, it is difficult to determine the number or size of stones in the gallbladder with transabdominal ultrasound. This is especially true for very small stones (1 or 2 mm in diameter) that frequently, when present in large numbers, can appear on transabdominal ultrasound as one large stone.
Next steps if the ultrasound is negative — For patients with symptoms that do not fit the classic description for biliary colic, an evaluation for non-biliary causes for the patient’s symptoms should be pursued. However, in a patient with classic biliary colic, if the initial transabdominal ultrasound was negative, additional testing to detect missed gallstones, sludge, or microlithiasis is indicated. (See ‘Differential diagnosis’ below.)
General approach — In patients with typical biliary colic but no gallstones on ultrasonography, we usually repeat the transabdominal ultrasound in a few weeks. If the repeat transabdominal ultrasound is negative, the patient may have microlithiasis or may be a category 4 patient (typical biliary symptoms without gallstones on ultrasound). In such patients the next step is debatable. The approach depends on the patient’s preferences, age, and risk factors for adverse outcomes with invasive procedures.
The more definitive approach is to proceed with endoscopic ultrasonography (EUS) to look for missed stones or sludge and, if the EUS is negative, obtain samples of bile for bile microscopy to evaluate for microlithiasis. However, some centers recommend cholecystokinin-stimulated cholescintigraphy before an EUS with bile sampling. Cholescintigraphy is more widely available and less invasive. A positive result (low gallbladder ejection fraction) suggests functional gallbladder disorder, though it may also be seen in the setting of microlithiasis or sludge and microcrystals that are interfering with bile ejection through the cystic duct. Differentiating between the two entities is typically not required since both conditions are treated with cholecystectomy. If the cholescintigraphy is normal, EUS can then be pursued. (See “Functional gallbladder disorder in adults”, section on ‘CCK-stimulated cholescintigraphy’ .)
If medical dissolution therapy with oral bile acids is being considered, EUS with bile collection for microscopy should be done first to confirm the presence of microlithiasis or sludge. Many patients with microlithiasis will respond to a one- to two-year course of oral bile acid therapy. (See “Dissolution therapy for the treatment of gallstones”, section on ‘Bile acid therapy’ .)
Repeat transabdominal ultrasound — Repeating the transabdominal ultrasound increases the sensitivity for detecting stones, particularly if they are smaller than 3 mm in diameter. A repeat examination should pay particular attention to regions of the gallbladder where stones are easily overlooked [ 34]. Patients with a negative repeat transabdominal ultrasound may still have microlithiasis or small stones that were missed. EUS and bile microscopy may identify missed stones or microlithiasis. These tests also both include an upper endoscopy, which also helps to exclude other conditions, such as peptic ulcer disease. If no stones are seen with EUS and bile microscopy, other disorders in the differential diagnosis of biliary colic (eg, sphincter of Oddi dysfunction or functional gallbladder disorder) should be considered. (See ‘Differential diagnosis’ below.)
It is important to thoroughly evaluate category 4 patients who have biliary colic but negative transabdominal ultrasounds because patients with missed stones or microlithiasis will typically respond to cholecystectomy. However, patients with other diagnoses, such as sphincter of Oddi dysfunction, peptic ulcer disease, dyspepsia, or irritable bowel syndrome, may not improve or may even worsen following cholecystectomy. (See “Clinical manifestations and diagnosis of sphincter of Oddi dysfunction” and “Approach to the patient with dyspepsia” and “Clinical manifestations and diagnosis of irritable bowel syndrome” and “Functional gallbladder disorder in adults” .)
Endoscopic ultrasound — Imaging of the gallbladder can be obtained by EUS. During EUS, an ultrasound transducer on the tip of an endoscope is placed into contact with the gastric antrum, which is in close proximity to the gallbladder. This permits gallbladder visualization without interference from bowel gas, subcutaneous tissue, or the liver. As a result, EUS is more sensitive than transabdominal ultrasound for the detection of gallstones, particularly in patients who are obese or have other anatomic considerations that limit gallbladder visualization with transabdominal ultrasound [ 35,36 ].
Several studies have demonstrated that EUS is useful for the detection of small stones and microlithiasis [ 35-38 ]. In one study of 45 patients in whom there was a clinical suspicion of cholelithiasis but with at least two normal transabdominal ultrasound examinations, EUS detected evidence of cholelithiasis in 26 patients (58 percent). The sensitivity and specificity of EUS for detecting cholelithiasis were 96 and 86 percent, respectively [ 35 ].
In a second study of 89 patients with acute pancreatitis, EUS revealed small gallbladder stones (1 to 9 mm) in 14 of 18 patients who had otherwise negative standard imaging studies, including transabdominal ultrasound [ 36 ]. Subsequent endoscopic retrograde cholangiopancreatography (ERCP) and cholecystectomy confirmed the presence of stones in all 14 patients. None of the remaining four patients developed evidence of cholelithiasis during a median follow-up of 22 months.
Bile microscopy — Bile microscopy detects microcrystals of cholesterol or amorphous bilirubinate as indirect evidence for the presence of microlithiasis in the bile. It has an overall sensitivity of 65 to 90 percent for identifying patients with gallstones [ 38-42 ]. Because of the improved sensitivity of transabdominal ultrasonography for detection of small stones and sludge, there is less need for microcrystal analysis. However, it still has a role in category 4 patients with biliary colic without gallstones on transabdominal ultrasound. However, because obtaining a sample for bile microscopy during endoscopy can take over 45 minutes, we reserve the procedure for patients with a negative EUS.
The test is based upon the theory that patients with cholesterol microlithiasis have bile that is supersaturated with cholesterol and thus have cholesterol monohydrate crystals in their gallbladder bile ( picture 1 ), while those with bilirubinate microlithiasis have amorphous reddish-brown bilirubinate granules in their gallbladders ( picture 2 ) [ 43,44 ]. However, the methods for performing the test have not been well standardized, which has led to confusion regarding how to collect and process the bile samples for analysis and what constitutes a positive test.
The proportion of patients with suspected gallstones but negative transabdominal ultrasound found to have microlithiasis varies substantially among reports. A systematic review found that microcrystals accounted for 7 to 79 percent of cases of idiopathic pancreatitis, 83 percent of patients with unexplained biliary-type pain, and 25 to 60 percent of patients with altered biliary and pancreatic sphincter function [ 45 ].
While the presence of any cholesterol crystals is theoretically abnormal, to increase specificity, some of the newer reports presume the test to be positive only if more than three crystals are seen per high power field [ 46 ]. However, whether findings based upon this approach correlate with clinical outcomes has not been established. As a result, this presumption has not been widely accepted.
Bile collection — Most available studies describe the test as it pertains to the detection of microlithiasis in patients with idiopathic recurrent pancreatitis and have used variable techniques for bile collection, bile processing, and microscopic crystal analysis. Nevertheless, most investigators agree that crystals are formed in the gallbladder where bile is concentrated, so gallbladder bile rather than hepatic bile should be analyzed [ 23,39,47 ]. Hepatic bile is significantly less concentrated and thus has a lower yield for the detection of microlithiasis.
Gallbladder bile can be collected using the following techniques:
- Through direct percutaneous puncture of the gallbladder under ultrasound or fluoroscopic guidance
- During endoscopic retrograde cholangiopancreatography, either through selective gallbladder cannulation or by aspirating bile from the common bile duct after stimulating gallbladder contraction with a slow intravenous infusion of the cholecystokinin (CCK) analogue, sincalide
- During endoscopy by suctioning bile from the duodenum in the region of the ampulla after gallbladder stimulation with sincalide
In most cases, collection during endoscopy is the simplest and most practical method. Since EUS includes an endoscopic examination, bile collection can be performed during the same session as an EUS, which increases the sensitivity for detecting gallstones over that of EUS alone [ 35,37 ]. (See ‘Endoscopic ultrasound’ above.)
Our approach in patients with biliary colic and a negative EUS is to collect a bile sample during the same endoscopic session as the EUS. Sincalide (0.03mcg/kg body weight) is given by intravenous drip over 45 minutes; the longer infusion is safer and more effective than a short bolus technique [ 48 ]. The tip of the endoscope is positioned next to the ampulla and the bile is aspirated. Bile flow usually starts to accelerate within five minutes of the start of the sincalide infusion. The first 5 to 10 minutes of bile flow is normally light in color and represents common bile duct and hepatic bile. Gallbladder bile is the darker bile that starts flowing several minutes later. We use a commercially available bile collecting catheter with a mushroom tip that we introduce through the working channel of the endoscope and connect to an external suction trap. Once we start to observe dark gallbladder bile being suctioned into the collecting trap, we empty the light colored bile from the trap and begin collecting the dark bile sample. When about 10 to 20 mL of bile has been collected, we stop the Sincalide infusion and conclude the procedure. This typically takes about 30 to 45 minutes from the start of the sincalide infusion to accomplish.
The darker bile is collected in a separate collecting tube and is incubated at 37 degrees C for 24 hours, then centrifuged at 3000 G for 30 minutes [ 49 ]. The supernatant is discarded and the sediment is mixed into the liquid remaining at the bottom of the tube. A drop of that liquid is placed on a slide and examined using a polarizing microscope; a polarizing filter facilitates identification of cholesterol crystals, which exhibit birefringence (they shine against the dark background of the polarizing microscope). The test is considered positive if any cholesterol crystals or amorphous red-brick colored bilirubinate granules are seen.
Tests that are rarely done
Oral cholecystography — Oral cholecystography can diagnose gallstones and assess gallbladder function, but it has largely been replaced by more sensitive and specific tests, such as transabdominal ultrasound [ 28,50 ]. It is still occasionally used in patients in whom a high quality ultrasound examination cannot be obtained (such as in obese patients), to confirm the presence of adenomyomatosis of the gallbladder, and to evaluate patients who are being considered for medical dissolution therapy with ursodeoxycholic acid , in whom it is important to demonstrate stone number and size, relative density of the stones to bile, cystic duct patency, and the gallbladder’s concentrating ability. (See “Patient selection for the nonsurgical treatment of gallstone disease” .)
An orally administered contrast agent (eg, iopanoic acid, sodium tyropanoate, or calcium ipodate) is given and is absorbed through the intestine, taken up by the liver, and secreted into bile. Gallstones appear as filling defects within the contrast on plain x-rays ( image 3 ). Non-opacification of the gallbladder can occur due to poor absorption from the intestine, impaired liver function, or extrahepatic biliary obstruction. With the currently available oral contrast agents, it is unlikely that the gallbladder will be visualized if the serum bilirubin is greater than 2 to 3 mg/dL.
An approximation of gallbladder motor function can also be obtained using oral cholecystography. The patient is given a fatty meal and serial x-rays are obtained. If the gallbladder is functioning normally, there will be a decrease in gallbladder size over time. Evaluation of the gallbladder motor function is not recommended in patients who have known gallbladder stones since it may induce biliary colic or complications of gallstone disease.
DIFFERENTIAL DIAGNOSIS — Many of the symptoms seen with uncomplicated gallstone disease may also be seen with other disorders or in patients who have developed complications from their gallstones. Hence, it is important to consider alternative diagnoses prior to making a diagnosis of uncomplicated gallstone disease.
Upper abdominal symptoms — Gallstone disease is usually considered as part of the differential diagnosis of patients presenting with upper abdominal symptoms. Other disorders in the differential diagnosis include:
- Esophageal chest pain
- Gastroesophageal reflux disease
- Peptic ulcer disease
- Nonulcer dyspepsia
- Hepatitis
- Functional gallbladder disorder
- Sphincter of Oddi dysfunction
- Chronic pancreatitis
- Irritable bowel syndrome
- Ischemic heart disease
- Pyelonephritis
- Ureteral calculi
- Complications of gallstone disease: acute cholecystitis, choledocholithiasis, acute pancreatitis, and acute cholangitis
It is important to remember that many of these diagnoses, such as irritable bowel syndrome, are common in the general population and thus may coexist with, but be unrelated to, gallstones. Because of this, an extensive search for gallstones in patients with nonspecific or atypical symptoms is discouraged. A general approach to the evaluation of patients with abdominal pain is discussed in detail elsewhere. (See “Diagnostic approach to abdominal pain in adults”and “Differential diagnosis of abdominal pain in adults” .)
An important feature for differentiating uncomplicated gallstone disease from non-biliary disorders is the presence of biliary colic, which has been shown to be predictive of the presence of gallstones on imaging [ 51,52 ]. However, biliary colic may be present in patients with other biliary disorders, such as acute cholecystitis, choledocholithiasis, sphincter of Oddi dysfunction, and functional gallbladder disorder. (See ‘Other disorders with biliary-type pain’below.)
Laboratory studies can be helpful for excluding other diagnoses and detecting complications of gallstone disease. The choice and order of testing varies depending upon the clinical presentation and suspicion for a particular diagnosis. Some commonly obtained tests include:
- Liver biochemical tests (serum aminotransferases, total bilirubin, alkaline phosphatase), which may be abnormal in patients with hepatitis, biliary tract obstruction, or (less often) acute cholecystitis (see “Approach to the patient with abnormal liver biochemical and function tests” )
- Serum amylase and lipase, which are elevated in acute pancreatitis
- Complete blood count, which may show an elevated white blood cell count in patients with acute cholecystitis or acute cholangitis
- Urine analysis, which may show evidence of a urinary tract infection or ureteral calculi
Other tests that may be indicated depending upon the patient’s symptoms and history include:
- Upper endoscopy to look for peptic ulcer disease
- Endoscopic ultrasonography to look for chronic pancreatitis
- Endoscopic retrograde cholangiopancreatography (ERCP) with sphincter of Oddi manometry to look for sphincter of Oddi dysfunction
- Cholescintigraphy with or without cholecystokinin (CCK)-stimulation to look for acute cholecystitis and functional gallbladder disorder, respectively
- Testing for ischemic heart disease
- Esophageal manometry to look for esophageal sources of chest pain, such as esophageal spasm
Other disorders with biliary-type pain — Patients with acute cholecystitis, choledocholithiasis, sphincter of Oddi dysfunction, and functional gallbladder disorder may all present with biliary colic. Acute cholecystitis and choledocholithiasis typically present acutely and patients often seek urgent medical attention. Sphincter of Oddi dysfunction and functional gallbladder disorder, on the other hand, may occur intermittently and may not be severe enough to prompt the patient to seek urgent evaluation.
Acute cholecystitis — Acute cholecystitis is the most common complication of gallstone disease and needs to be differentiated from uncomplicated gallstone disease in patients presenting with biliary colic. An episode of prolonged right upper quadrant pain (greater than four to six hours), especially if associated with fever, should arouse suspicion for acute cholecystitis as opposed to an attack of simple biliary colic. (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis” .)
Physical examination can help differentiate uncomplicated gallstone disease from acute cholecystitis. While biliary colic is present in both uncomplicated gallstone disease and in acute cholecystitis, the pain in uncomplicated gallstone disease is entirely visceral in origin since the gallbladder wall is not inflamed. Thus, it is less well localized and patients do not exhibit a positive Murphy’s sign on physical examination. A Murphy’s sign is elicited by palpating the area of the gallbladder fossa just beneath the liver edge while the patient is asked to inspire deeply, causing the gallbladder to descend toward the examining fingers. Patients with acute cholecystitis commonly experience increased discomfort and may have an associated inspiratory arrest (a positive Murphy’s sign). (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis” .)
Laboratory tests should be normal in patients with uncomplicated gallstone disease. On the other hand, patients with acute cholecystitis may have a leukocytosis and mild elevations in serum aminotransferases, bilirubin, and amylase. Transabdominal ultrasound findings that are not seen in patients with uncomplicated gallstone disease but that may be present with acute cholecystitis include gallbladder wall thickening or edema and a “sonographic Murphy’s sign” in which pain is reproduced when the gallbladder is compressed by the ultrasound probe under direct ultrasonic visualization. Cholescintigraphy (99mTc-heapto-iminodiacetic acid [HIDA] scanning) is not used in the diagnosis of gallstones, but is useful in excluding acute cholecystitis in patients who present with acute biliary colic. (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis”, section on ‘Diagnosis’ .)
A detailed discussion of the approach to patients with suspected acute cholecystitis is presented elsewhere. (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis” and “Treatment of acute cholecystitis” .)
Choledocholithiasis — Patients with a stone in the common bile duct (choledocholithiasis) may have typical biliary colic. However, the pain is usually more prolonged than is seen with uncomplicated gallstone disease. Serum aminotransferases are normal with uncomplicated gallstone disease but are typically elevated early in the course of biliary obstruction. If the stone is not passed, a cholestatic pattern develops (increased bilirubin, alkaline phosphatase, and gamma-glutamyl transpeptidase out of proportion to the elevation in the aminotransferases). Patients who have developed acute cholangitis may also present with fever, leukocytosis, hypotension, or mental status changes. (See “Approach to the patient with suspected choledocholithiasis”, section on ‘Laboratory evaluation’ and “Acute cholangitis”, section on ‘Clinical manifestations’ .)
Transabdominal ultrasound may reveal a stone in the common bile duct, but the sensitivity is poor for stones in the distal common bile duct. A dilated common bile duct supports a diagnosis of choledocholithiasis, but is not specific. Magnetic resonance cholangiopancreatography, endoscopic ultrasound, or ERCP may be required to confirm the diagnosis, and in the case of ERCP, provide therapy. (See “Approach to the patient with suspected choledocholithiasis”, section on ‘Imaging tests’ .)
The approach to the diagnosis and management of patients with choledocholithiasis is discussed in detail elsewhere. (See “Approach to the patient with suspected choledocholithiasis” .)
Sphincter of Oddi dysfunction — The term sphincter of Oddi dysfunction (SOD) has been used to describe a clinical syndrome of biliary or pancreatic obstruction related to mechanical or functional abnormalities of the sphincter of Oddi. Patients with SOD may have biliary colic that lasts from about 30 minutes to several hours. Unlike patients with uncomplicated gallstone disease, patients with SOD may have elevations in their aminotransferases, alkaline phosphatase, amylase, or lipase. In addition, the common bile duct may appear dilated on transabdominal ultrasound. In some cases, sphincter of Oddi manometry may be required to confirm the diagnosis of SOD.
The approach to patients with suspected Sphincter of Oddi is discussed in detail elsewhere. (See “Clinical manifestations and diagnosis of sphincter of Oddi dysfunction” and “Treatment of sphincter of Oddi dysfunction” .)
Functional gallbladder disorder — Functional gallbladder disorder is a diagnosis of exclusion. Patients with functional gallbladder disorder have biliary colic, but do not have gallstones, sludge, or microlithiasis. To differentiate functional gallbladder disorder from uncomplicated gallstone disease, patients must have a thorough evaluation for gallstones and other disorders that may cause upper abdominal symptoms. If this testing is negative, patients then undergo CCK-stimulated cholescintigraphy to determine the gallbladder ejection fraction, which is low in patients with functional gallbladder disorder. (See “Functional gallbladder disorder in adults”, section on ‘CCK-stimulated cholescintigraphy’ .)
Functional gallbladder disorder is discussed in detail elsewhere. (See “Functional gallbladder disorder in adults” .)
MANAGEMENT — The approach to the management of patients with gallstones depends upon the patient’s symptoms, imaging test findings, and whether complications are present. In general, patients with sludge or microlithiasis are managed the same as patients with gallstones. Most asymptomatic patients are followed expectantly, whereas patients with recurrent severe symptoms are treated with pain control and cholecystectomy. The management of patients with atypical or mild symptoms and gallstones or with typical biliary colic but no gallstones is more complicated and may include empiric treatments for other disorders or, in appropriately selected patients, cholecystectomy.
We have found it useful to divide patients into four categories to help guide management:
- Category 1: Patients with gallstones but no symptoms
- Category 2: Patients with typical biliary symptoms and gallstones
- Category 3: Patients with gallstones but atypical symptoms
- Category 4: Patients with typical biliary symptoms but without gallstones on ultrasound
The management of patients with complications due to gallstones is discussed separately. (See “Treatment of acute cholecystitis” and “Approach to the patient with suspected choledocholithiasis”, section on ‘Approach to diagnosis and management’ and “Treatment of acute pancreatitis” and “Acute cholangitis” and “Gallstone ileus”, section on ‘Treatment’ and “Mirizzi syndrome”, section on ‘Treatment’ and “Surgical management of gallbladder cancer”and “Adjuvant treatment for localized, potentially resectable gallbladder cancer” and “Treatment of advanced, unresectable gallbladder cancer” .)
Category 1 patients (gallstones but no symptoms) — Most patients who are asymptomatic but found to have incidental gallstones on an imaging test do not require treatment since the risk of developing life-threatening, severe complications is low. This recommendation is based upon studies showing that the rate of progression from asymptomatic to symptomatic gallstones is very low (about 1 percent per year). In addition, when patients do become symptomatic, the initial presenting symptoms are usually not severe, allowing for cholecystectomy at that time. As a result, most patients with incidental gallstones can be educated about potentially concerning symptoms, so they may seek medical attention before severe complications arise. (See “Approach to the patient with incidental gallstones” .)
However, some patients may be at increased risk for complications or cancer, and in such patients prophylactic cholecystectomy may be warranted. (See”Approach to the patient with incidental gallstones”, section on ‘Patients at increased risk of complications’ .)
Some data suggest that physical activity may reduce the risk of developing symptomatic gallstone disease. In a study of more than 60,000 women, women who were seated for less than six hours per week were less likely to undergo cholecystectomy compared with those who sat for 41 to 60 hours or more than 60 hours (relative risks 1.4 and 2.3, respectively) [ 53 ]. In a second study, there was a three-fold increase in gallstone disease among men who watched television for more than 40 hours per week compared with those who watched for less than six hours per week [ 54 ].
Category 2 patients (typical biliary symptoms and gallstones) — In patients with a classic presentation of uncomplicated gallstone disease there are two general considerations when it comes to management:
- Acute management of biliary colic.
- Prophylactic treatment: In contrast to patients with incidental gallstones, prophylactic treatment to remove the offending stones (typically by cholecystectomy) is recommended for patients with gallstone disease, both to prevent future attacks of biliary colic and to prevent the complications of gallstone disease. Whether to perform prophylactic cholecystectomy in patients with mild symptoms depends upon factors such as the patient’s age, comorbid illnesses, and the frequency of attacks. (See ‘Natural history’ above.)
Pain management — During an acute attack of biliary colic, management is focused on pain control. Pain control can usually be achieved with nonsteroidal antiinflammatory drugs (NSAIDs) or opioids. Those with prolonged attacks (especially if accompanied by vomiting) should also receive intravenous hydration.
We prefer ketorolac (30 to 60 mg adjusted for age and renal function given in a single intravenous or intramuscular dose) for patients who present to the emergency department with biliary colic. Treatment usually relieves symptoms within 10 to 30 minutes. Patients are then prescribed ibuprofen 400 mg orally for subsequent attacks that may occur while the patient is awaiting cholecystectomy. We reserve opioids for patients who have contraindications to NSAIDs or who do not achieve adequate pain relief with an NSAID.
The role for NSAIDs in the treatment of biliary colic was demonstrated in a meta-analysis of 11 randomized trials with 1076 patients that compared NSAIDs with no treatment, placebo, or other treatments [ 55 ]. NSAIDs were more likely to control pain than placebo (relative risk [RR] 3.8; 95% confidence interval [CI] 1.7-8.6) or antispasmodics (RR 1.5; 95% CI 1.0-2.1). In addition, there was no difference in pain control between NSAIDs and opioids (RR 1.1; 95% CI 0.8-1.3). NSAIDs may also favorably alter the natural history of biliary colic, possibly due to the role of prostaglandins in the development of acute cholecystitis [ 56,57 ]. (See “Pathogenesis, clinical features, and diagnosis of acute cholecystitis”, section on ‘Pathogenesis’ .)
Opioids, such as morphine , hydromorphone , or meperidine , are an alternative for patients who cannot take NSAIDs or who fail to respond to an NSAID. It has traditionally been taught that meperidine is the narcotic of choice in patients with biliary colic or gallstone pancreatitis because it has less of an effect on sphincter of Oddi motility than morphine [ 58-60 ]. However, a systematic review found that all opioids result in increased sphincter of Oddi pressure when measured using sphincter of Oddi manometry [ 59 ]. In addition, there are no clinical studies comparing meperidine and morphine, nor are there clinical studies to suggest that morphine causes pancreatitis or cholecystitis. Thus, there are insufficient data to suggest that morphine should be avoided in patients with biliary colic. In addition, morphine has the benefit of having a longer half-life than meperidine. Meperidine’s short half-life may lead to the need for frequent dosing, resulting in the accumulation of the metabolite normeperidine, which causes neuromuscular irritation and, rarely, seizures.
While anticholinergic agents are useful in the management of renal colic due to their smooth muscle relaxation effects, they do not appear to help biliary colic [ 61 ].
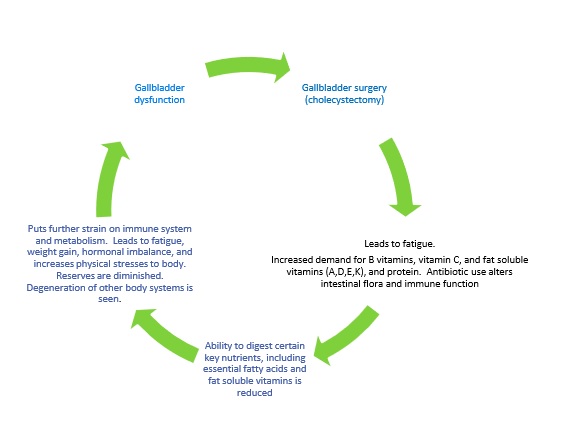
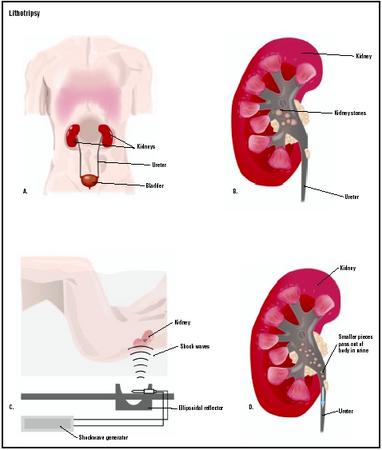
Cholecystectomy — Definitive prophylactic therapy to prevent future attacks of biliary colic and to prevent the complications of gallstone disease is appropriate for patients with recurrent attacks of moderate or severe biliary colic, or with an isolated severe attack. Several modalities are available ranging from cholecystectomy to medical dissolution of the stones. Cholecystectomy is recommended for the majority of patients, but medical dissolution or extracorporeal shock-wave lithotripsy therapy may be appropriate for patients who are poor surgical candidates. (See “Dissolution therapy for the treatment of gallstones”, section on ‘Medical gallstone dissolution’ and “Open cholecystectomy” and “Laparoscopic cholecystectomy: Techniques” .)
The approach to treatment is not as clear for patients with isolated or recurrent attacks of mild biliary colic. Such patients are at low risk for developing complications (one to two percent per year). The decision to proceed with prophylactic cholecystectomy in such patients should take into account factors such as the patient’s age (younger patients are more likely to develop complications due to their longer life-expectancy), the frequency of the attacks (with more frequent attacks favoring prophylactic therapy), the patient’s surgical risk, and the patient’s attitudes toward surgery and expectant management (eg, some patients may be more concerned about a severe complication than undergoing a surgical procedure, whereas others may prefer to avoid surgery and are willing to accept the risk of developing a gallstone-related complication). Another option for patients in this group that we frequently offer is oral dissolution therapy with bile acids. Studies suggest that long-term ursodeoxycholic acid therapy of 600 mg per day reduces the risk of biliary complications and the need for a cholecystectomy by 30 percent [ 62 ]. (See “Dissolution therapy for the treatment of gallstones”, section on ‘Bile acid therapy’ .)
Surgical approach — Cholecystectomy is typically preformed laparoscopically, though it may also be performed through an open right upper quadrant incision. A laparoscopic approach eliminates the need to cut the rectus abdominis muscle and is associated with less postoperative pain, better cosmesis, shorter hospital stays, and less time off from work than open cholecystectomy [ 63-67 ]. However, the laparoscopic procedure has been associated with an increased risk of common bile duct injury [ 68,69 ]. In addition, the laparoscopic procedure may require conversion to an open procedure due to a variety of technical or patient issues. (See “Complications of laparoscopic cholecystectomy” .)
Efficacy — While patients with biliary colic and gallstones on imaging usually respond well to cholecystectomy, it is not always curative. In a systematic review of 23 studies looking at the effect of cholecystectomy for patients with gallstones, 92 percent of patients with biliary colic had symptom relief following cholecystectomy [ 11 ].
Factors that predict a response to cholecystectomy were evaluated in a study of 1008 patients with upper abdominal pain and gallstones [ 70 ]. Upper abdominal pain relief was reported by 594 patients (59 percent) following cholecystectomy. On multivariable analysis, factors associated with pain relief following cholecystectomy included pain that occurred once a month or less (odds ratio [OR] 1.6), pain that began one year or less prior to surgery (OR 1.3), and pain that awakened the patient at night (OR 1.5). Factors associated with a lower likelihood of achieving pain relief were the presence of lower abdominal pain (OR 0.7), usually having an abnormal bowel pattern (OR 0.6), and often feeling bloated or “burpy” (OR 0.6).
Complications and side effects — Major complications have been reported to occur in 2.6 percent of laparoscopic cholecystectomies and include bleeding, abscess formation, bile leak, biliary injury, and bowel injury. (See “Complications of laparoscopic cholecystectomy” .)
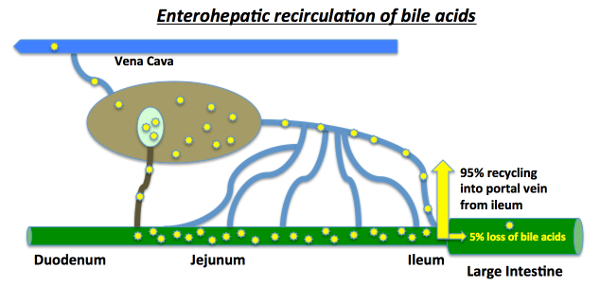
While removal of the gallbladder is commonly considered to have no lasting physiologic consequences, 5 to 12 percent of patients develop diarrhea, though in many cases the diarrhea will improve or resolve over weeks to months. Increased risks of right sided colon cancer, esophageal cancer, and small intestinal cancer in patients who have undergone cholecystectomy have also been suggested [ 71-73 ]. This may be related to the effects of increased concentrations of the bile acid deoxycholic acid in the gut lumen as a result of loss of the gallbladder, which normally acts as a reservoir for concentrated bile acids. (See “Approach to the adult with chronic diarrhea in developed countries”, section on ‘Cholecystectomy’ and “Colorectal cancer: Epidemiology, risk factors, and protective factors”, section on ‘Cholecystectomy’ .)
Alternatives to cholecystectomy — In some cases, surgical removal of the gallbladder may not be feasible, usually because of patient comorbidities. Several nonsurgical techniques for treatment of gallstones have been developed. These include medical dissolution therapy with oral bile acids and extracorporeal shock-wave lithotripsy. While the development of laparoscopic cholecystectomy has generally reduced enthusiasm for these approaches, they remain reasonable options in selected patients. (See “Patient selection for the nonsurgical treatment of gallstone disease” and”Dissolution therapy for the treatment of gallstones” .)
Category 3 patients (gallstones but atypical symptoms) — Some patients with atypical symptoms and gallstones respond to cholecystectomy, but the response rates are lower than those seen for patients with typical biliary colic. This suggests that in some patients, the atypical symptoms are related to the gallstones, but that in others they are due to another cause and the gallstones are an incidental finding. Thus, a careful search for other causes of a patient’s atypical symptoms is indicated. However, symptoms as described by patients are highly subjective and often change. As a result, it is useful to review the symptoms on more than one occasion to see if a patient has developed biliary colic. (See ‘Differential diagnosis’ above.)
The probability of patients with atypical symptoms and gallstones responding to cholecystectomy was evaluated in a systematic review. Among patients with upper abdominal pain (but not necessarily biliary colic), the relief rates for elective and acute cholecystectomy were 72 and 86 percent, respectively. In patients with dyspeptic symptoms, the relief rates were 56 and 82 percent, respectively. In addition, 65 percent of patients with food intolerance reported relief after 12 months.
An empiric trial of oral dissolution therapy with ursodeoxycholic acid (UDCA) may help identify patients who will benefit from cholecystectomy, provided there has been a thorough evaluation for other causes of the symptoms. UDCA therapy relieves the symptoms in many patients within three months if the symptoms are due to gallstones [ 74 ]. While UDCA therapy may provide symptomatic relief, the rates of complete stone dissolution are poor (37 percent in a meta-analysis), leaving patients at risk for complications from their gallstones [ 75 ]. As a result, we refer patients who respond to UDCA for cholecystectomy if they are surgical candidates, especially if they are not interested in staying on UDCA for two to three years to see if their stones will dissolve. We do not suggest cholecystectomy in patients who fail to respond to UDCA, and instead treat for disorders more consistent with the patient’s symptoms (eg, functional dyspepsia in a patient with bloating). (See “Dissolution therapy for the treatment of gallstones” and “Functional dyspepsia”, section on ‘Treatment’ .)
Category 4 patients (typical biliary symptoms but without gallstones on ultrasound) — Patients with biliary colic but no gallstones or other non-biliary causes for the pain detected after a thorough evaluation may have functional gallbladder disorder. If cholecystokinin-stimulated cholescintigraphy reveals a low gallbladder ejection fraction, a finding that is suggestive of functional gallbladder disorder, the appropriate treatment is cholecystectomy. However, if the evaluation for functional gallbladder disorder is negative, patients are generally treated for functional dyspepsia or irritable bowel syndrome. (See “Functional dyspepsia”, section on ‘Treatment’ and “Treatment of irritable bowel syndrome” .)
Patients with gallstone-related complications — The complications of cholelithiasis include acute cholecystitis, choledocholithiasis, gallstone pancreatitis, acute cholangitis, gallstone ileus, Mirizzi syndrome, and gallbladder cancer. The management of these complications is discussed in detail elsewhere. (See “Treatment of acute cholecystitis” and “Approach to the patient with suspected choledocholithiasis”, section on ‘Approach to diagnosis and management’ and “Treatment of acute pancreatitis” and “Acute cholangitis” and “Gallstone ileus”, section on ‘Treatment’ and “Mirizzi syndrome”, section on ‘Treatment’ and “Surgical management of gallbladder cancer” and “Adjuvant treatment for localized, potentially resectable gallbladder cancer” and”Treatment of advanced, unresectable gallbladder cancer” .)
Women with gallstones who are pregnant — The approach to women with gallstones who are pregnant is discussed in detail elsewhere. (See”Gallstone disease in pregnant women” .)
INFORMATION FOR PATIENTS — UpToDate offers two types of patient education materials, “The Basics” and “Beyond the Basics.” The Basics patient education pieces are written in plain language, at the 5 th to 6 th grade reading level, and they answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on “patient info” and the keyword(s) of interest.)
- Basics topics (see “Patient information: Gallstones (The Basics)” and “Patient information: Gallbladder removal (cholecystectomy) (The Basics)” )
- Beyond the Basics topics (see “Patient information: Gallstones (Beyond the Basics)” )
SUMMARY AND RECOMMENDATIONS
- Patients with uncomplicated gallstone disease typically present with biliary colic, normal physical examination findings, and normal laboratory test results. Biliary colic is often associated with diaphoresis, nausea, and vomiting. (See ‘Clinical features’ above.)
- Complications from asymptomatic gallstones occur at a rate of approximately one to two percent per year but are more common in patients with symptomatic gallstones. Complications include acute cholecystitis, choledocholithiasis with or without acute cholangitis, and gallstone pancreatitis. Rare complications include gallbladder cancer, gallstone ileus, and Mirizzi syndrome. (See ‘Natural history’ above.)
- Typically, the evaluation of a patient with biliary colic begins with a transabdominal ultrasound. If the ultrasound is negative, additional studies that may help with the diagnosis include repeating the transabdominal ultrasound, endoscopic ultrasound, and bile microscopy. (See ‘Diagnosis’ above.)
- Patients with uncomplicated gallstone disease may have ultrasound findings of gallstones, gravel, or sludge. Distinguishing among these three entities is generally not clinically important because they are managed identically. On ultrasound, gallstones appear as echogenic foci that cast an acoustic shadow ( image 2 ) and seek gravitational dependency. Gravel is the appearance of multiple small stones that are echogenic and cast shadows. Sludge, which represents cholesterol crystals and bilirubinate particles in a mucus glycoprotein gel, is echogenic in appearance but does not cast an acoustic shadow. (See ‘Transabdominal ultrasound’ above.)
- Gallstone disease is usually considered as part of the differential diagnosis of patients presenting with upper abdominal symptoms. Thus, the decision to implicate the gallbladder has to be made based upon clinical suspicion for a varied group of disorders that include peptic ulcer disease, nonulcer dyspepsia, functional gallbladder disorder, sphincter of Oddi dysfunction, and ischemic heart disease. In addition, complications related to gallstones, such as acute cholecystitis, choledocholithiasis, pancreatitis, and acute cholangitis also need to be considered. (See ‘Differential diagnosis’ above.)
- The approach to management of patients with uncomplicated gallstones or simple biliary colic depends upon the patient’s symptoms and imaging test findings. We have found it useful to divide patients into four categories to help guide management:
- Category 1: Patients with gallstones but no symptoms
- Category 2: Patients with typical biliary symptoms and gallstones
- Category 3: Patients with gallstones but atypical symptoms
- Category 4: Patients with typical biliary symptoms but without gallstones on ultrasound
- Category 1 : The majority of patients with asymptomatic (incidental) gallstones do not require treatment because they are unlikely to develop symptoms and, if symptoms do occur, they are generally mild initially. However, patients must be educated about the symptoms of gallstone disease so they can seek treatment before more severe symptoms or complications develop. On the other hand, cholecystectomy may be a reasonable alternative in patients at increased risk for complications or gallbladder cancer. (See “Approach to the patient with incidental gallstones” .)
- Category 2 : For patients with recurrent attacks of moderate or severe biliary colic, or with an isolated severe attack, and gallstones on imaging, we recommend cholecystectomy rather than expectant management ( Grade 1B ). Such patients are likely to have recurrent attacks and are at risk for complications. Dissolution therapy or extracorporeal shock-wave lithotripsy is a reasonable alternative in patients who are not surgical candidates. (See ‘Category 2 patients (typical biliary symptoms and gallstones)’ above.)
Options for treating patients with mild symptoms include expectant management, prophylactic cholecystectomy, and oral dissolution therapy with bile acids. The choice of therapy will depend on factors such as the patient’s age (younger patients are more likely to develop complications due to their longer life-expectancy), the frequency of the attacks (with more frequent attacks favoring prophylactic therapy), the patient’s surgical risk, and the patient’s attitudes toward surgery and expectant management.
- Category 3 : For patients with atypical symptoms and gallstones, we suggest additional evaluation rather than cholecystectomy ( Grade 2C ). Such patients should be thoroughly evaluated for non-gallstone-related causes of their symptoms. Cholecystectomy is a reasonable alternative if a thorough evaluation for other causes of the patient’s symptoms is negative and if the patient has a symptomatic response to dissolution therapy withursodeoxycholic acid . (See ‘Category 3 patients (gallstones but atypical symptoms)’ above and ‘Differential diagnosis’ above.)
- Category 4 : Patients with biliary colic but no gallstones detected after a thorough evaluation for both biliary and non-biliary causes of their pain should be evaluated for functional gallbladder disorder, as patients with functional gallbladder disorder often respond to cholecystectomy. If the evaluation for functional gallbladder disorder is negative, patients are generally treated for functional dyspepsia or irritable bowel syndrome. (See’Category 4 patients (typical biliary symptoms but without gallstones on ultrasound)’ above and “Functional gallbladder disorder in adults” and”Functional dyspepsia”, section on ‘Treatment’ and “Treatment of irritable bowel syndrome” .)
- The management of patients with gallstone-related complications (eg, acute cholecystitis, gallstone pancreatitis, or acute cholangitis) is discussed in detail elsewhere. (See “Treatment of acute cholecystitis” and “Approach to the patient with suspected choledocholithiasis”, section on ‘Approach to diagnosis and management’ and “Treatment of acute pancreatitis” and “Acute cholangitis” and “Gallstone ileus”, section on ‘Treatment’ and “Mirizzi syndrome”, section on ‘Treatment’ and “Surgical management of gallbladder cancer” and “Adjuvant treatment for localized, potentially resectable gallbladder cancer” and “Treatment of advanced, unresectable gallbladder cancer” .)

 Gastroparesis, also called delayed gastric emptying, is a disorder in which the stomach takes too long to empty its contents. Normally, the stomach contracts to move food down into the small intestine for digestion. The vagus nerve controls the movement of food from the stomach through the digestive tract. Gastroparesis occurs when the vagus nerve is damaged and the muscles of the stomach and intestines do not work normally. Food then moves slowly or stops moving through the digestive tract.
Gastroparesis, also called delayed gastric emptying, is a disorder in which the stomach takes too long to empty its contents. Normally, the stomach contracts to move food down into the small intestine for digestion. The vagus nerve controls the movement of food from the stomach through the digestive tract. Gastroparesis occurs when the vagus nerve is damaged and the muscles of the stomach and intestines do not work normally. Food then moves slowly or stops moving through the digestive tract.

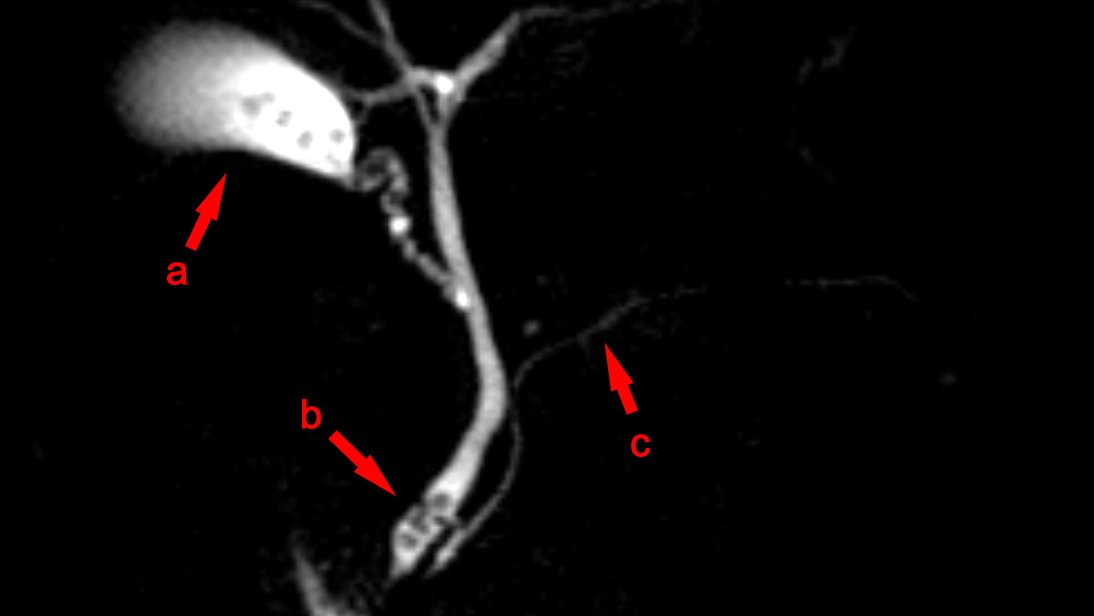
![choledocholithiasis-obstructive-jaundice-7-638[1]](http://lifewithnogallbladder.com/wp-content/uploads/2017/12/choledocholithiasis-obstructive-jaundice-7-6381.jpg)

 The cystic duct connects the top of the gallbladder’s neck to the common hepatic duct. It then joins the common bile duct, which meets pancreatic duct before it empties into the duodenum. In the average adult, the cystic duct measures four centimeters in length.
The cystic duct connects the top of the gallbladder’s neck to the common hepatic duct. It then joins the common bile duct, which meets pancreatic duct before it empties into the duodenum. In the average adult, the cystic duct measures four centimeters in length.