Role of Bile Acids In Digestion
Bile is a complex fluid containing water, electrolytes and a battery of organic molecules including bile acids, cholesterol, phospholipids and bilirubin that flows through the biliary tract into the small intestine. There are two fundamentally important functions of bile in all species:
Bile contains bile acids, which are critical for digestion and absorption of fats and fat-soluble vitamins in the small intestine.
Many waste products, including bilirubin, are eliminated from the body by secretion into bile and elimination in feces.
Adult humans produce 400 to 800 ml of bile daily, and other animals proportionately similar amounts. The secretion of bile can be considered to occur in two stages:
Initially, hepatocytes secrete bile into canaliculi, from which it flows into bile ducts. This hepatic bile contains large quantities of bile acids, cholesterol and other organic molecules.
As bile flows through the bile ducts it is modified by addition of a watery, bicarbonate-rich secretion from ductal epithelial cells.
In species with a gallbladder (man and most domestic animals except horses and rats), further modification of bile occurs in that organ. The gall bladder stores and concentrates bile during the fasting state. Typically, bile is concentrated five-fold in the gall bladder by absorption of water and small electrolytes – virtually all of the organic molecules are retained.
Secretion into bile is a major route for eliminating cholesterol. Free cholesterol is virtually insoluble in aqueous solutions, but in bile, it is made soluble by bile acids and lipids like lecithin. Gallstones, most of which are composed predominantly of cholesterol, result from processes that allow cholesterol to precipitate from solution in bile.
Role of Bile Acids in Fat Digestion and Absorption
Bile acids are derivatives of cholesterol synthesized in the hepatocyte. Cholesterol, ingested as part of the diet or derived from hepatic synthesis is converted into the bile acids cholic and chenodeoxycholic acids, which are then conjugated to an amino acid (glycine or taurine) to yield the conjugated form that is actively secreted into cannaliculi.
Bile acids are facial amphipathic, that is, they contain both hydrophobic (lipid soluble) and polar (hydrophilic) faces. The cholesterol-derived portion of a bile acid has one face that is hydrophobic (that with methyl groups) and one that is hydrophilic (that with the hydroxyl groups); the amino acid conjugate is polar and hydrophilic.
Their amphipathic nature enables bile acids to carry out two important functions:
Emulsification of lipid aggregates: Bile acids have detergent action on particles of dietary fat which causes fat globules to break down or be emulsified into minute, microscopic droplets. Emulsification is not digestion per se, but is of importance because it greatly increases the surface area of fat, making it available for digestion by lipases, which cannot access the inside of lipid droplets.
Solubilization and transport of lipids in an aqueous environment: Bile acids are lipid carriers and are able to solubilize many lipids by forming micelles – aggregates of lipids such as fatty acids, cholesterol and monoglycerides – that remain suspended in water. Bile acids are also critical for transport and absorption of the fat-soluble vitamins.
Role of Bile Acids in Cholesterol Homeostasis
Hepatic synthesis of bile acids accounts for the majority of cholesterol breakdown in the body. In humans, roughly 500 mg of cholesterol are converted to bile acids and eliminated in bile every day. This route for elimination of excess cholesterol is probably important in all animals, but particularly in situations of massive cholesterol ingestion.
Interestingly, it has recently been demonstrated that bile acids participate in cholesterol metabolism by functioning as hormones that alter the transcription of the rate-limiting enzyme in cholesterol biosynthesis.
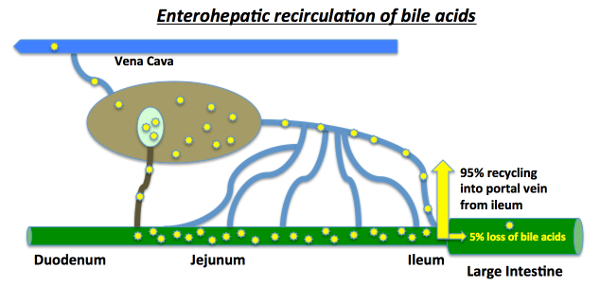
Enterohepatic Recirculation
Large amounts of bile acids are secreted into the intestine every day, but only relatively small quantities are lost from the body. This is because approximately 95% of the bile acids delivered to the duodenum are absorbed back into blood within the ileum.
Venous blood from the ileum goes straight into the portal vein, and hence through the sinusoids of the liver. Hepatocytes extract bile acids very efficiently from sinusoidal blood, and little escapes the healthy liver into systemic circulation. Bile acids are then transported across the hepatocytes to be resecreted into canaliculi. The net effect of this enterohepatic recirculation is that each bile salt molecule is reused about 20 times, often two or three times during a single digestive phase.
It should be noted that liver disease can dramatically alter this pattern of recirculation – for instance, sick hepatocytes have decreased ability to extract bile acids from portal blood and damage to the canalicular system can result in escape of bile acids into the systemic circulation. Assay of systemic levels of bile acids is used clinically as a sensitive indicator of hepatic disease.
Pattern and Control of Bile Secretion
The flow of bile is lowest during fasting, and a majority of that is diverted into the gallbladder for concentration. When chyme from an ingested meal enters the small intestine, acid and partially digested fats and proteins stimulate secretion of cholecystokinin and secretin. As discussed previously, these enteric hormones have important effects on pancreatic exocrine secretion. They are both also important for secretion and flow of bile:
Cholecystokinin: The name of this hormone describes its effect on the biliary system – cholecysto = gallbladder and kinin = movement. The most potent stimulus for release of cholecystokinin is the presence of fat in the duodenum. Once released, it stimulates contractions of the gallbladder and common bile duct, resulting in delivery of bile into the gut.
Secretin: This hormone is secreted in response to acid in the duodenum. Its effect on the biliary system is very similar to what was seen in the pancreas – it simulates biliary duct cells to secrete bicarbonate and water, which expands the volume of bile and increases its flow out into the intestine.
Source: http://www.vivo.colostate.edu/hbooks/pathphys/digestion/liver/bile.html