The Postcholecystectomy Syndrome (PCS): is a heterogeneous group of diseases and symptoms presenting following gallbladder removal. Symptoms occur in about 5 to 40 percent of patients who undergo cholecystectomy, and can be transient, persistent or lifelong. The chronic condition is diagnosed in approximately 10% of postcholecystectomy cases.
Post-cholecystectomy Syndrome may include:
- Diarrhoea as a troublesome problem range from 9 to 12% of which bile acid malabsorption (BAM) , 65% of these patients. [1]
- Depression disorders occurring in 0.9%-3.0% of patients[2]
- Bile (duodenogastric) reflux occurring in 20%-30% of patients[3,4,5]. Likely damage attributable to chronic bile exposure post-cholecystectomy includes:
- cellular damage to esophagogastric junction
- bile induced Gastroesophageal Mucosal Injury (Protective barrier that constrains the acidic reflux)
- increase the incidence of gastric and esophageal cancer
- Sphincter of Oddi dysfunction (SOD) is seen in 1% of patients after cholecystectomy, but in 14%-23% of patients with the post-cholecystectomy syndrome [6]
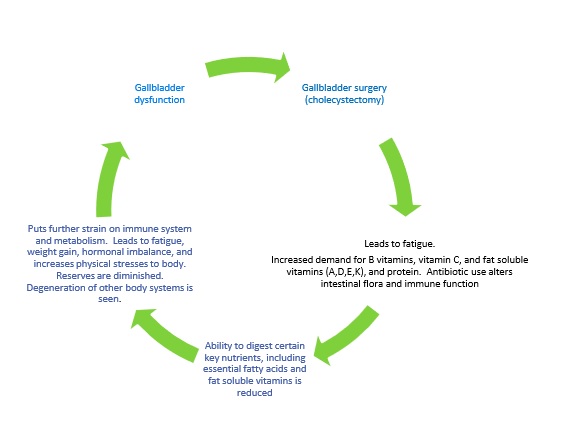
- increased Body Mass Index (weight gain) with metabolic syndrome, gastritis, liposoluble vitamin deficiency. Cholecystectomy can have nutritional and metabolic consequences and in the long-term[7]
The onset of symptoms may range from 2 days to 25 years. There may also be gender-specific risk factors for developing symptoms after cholecystectomy. In one study, the incidence of recurrent symptoms among female patients was 43%, compared to 28% of male patients.”
Patients with cholecystectomy had more comorbidities, particularly chronic fatigue syndrome, fibromyalgia, depression, and anxiety. Postcholecystectomy gastroparesis patients had increased health care utilization and had a worse quality of life.
Postcholecystectomy Syndrome in more detail
Absence of the gallbladder leads to development of functional biliary hypertension and dilatation of common bile duct and the common hepatic duct. The dilatation of right and left hepatic ducts may be formed within 3-5 years after cholecystectomy. Functional hypertension in the common bile duct leads to development of functional hypertension in Wirsung’s pancreatic duct accompanied by chronic pancreatitis symptoms.
During this period in some patients this is accompanied by chronic pancreatitis progression, dysfunction of the sphincter of Oddi and duodeno-gastral reflux. Duodeno-gastral reflux causes the development of atrophic (bile-acid-dependent) antral gastritis . After cholecystectomy 40% to 60% of patients suffer from dyspeptic disorders, 5% to 40% from pains of different localizations. Up to 70% of patients show symptoms of chronic “bland” intrahepatic cholestasis, chronic cholestatic hepatitis and compensatory bile-acid-dependent apoptosis of hepatocytes. In some of cholecystectomized patients with high concentration of hydrophobic hepatotoxic co-cancerogenic deoxycholic bile acid in serum and/or feces high risk of the colon cancer is found.
Not disclosed to patients, specialist medical opinion and studies list the following expected risks, side effects, diseases, syndromes and conditions after the removal of the gallbladder and its function. The majority of these problems are not accepted by the HDC as a risk and are blocked from disclosure to patients during the informed consent process, or advised during post-operative follow-ups.
They are but not exclusive to:
| Anatomy | Etiology |
| Biliary track | Biliary injury Cholangitis Choledochoduodenal fistula Choledocholithiasis Clip migration / Inaccurate clip placement Dyskinesia Nonspecific dilatation or hypertension Obstruction Strictures Stump cholelithiasis Adhesions Cyst Dilation without obstruction Fistula Hypertension or nonspecific dilation Malignancy and cholangiocarcinoma Trauma |
| Bone | Arthritis |
| Colon | Adhesions; incisional hernia; irritable bowel diseaseConstipationDiarrhoea Incisional hernia |
| Duodenum | AdhesionsDuodenal diverticulaIrritable bowel disease Peptic ulcer disease Perforation |
| Esophagus | AchalasiaAerophagiaDiaphragmatic hernia Esophagitis Hiatal hernia |
| Gallbladder and cystic Duct remnant | InflammationLeakMirizzi’s syndrome Mucocele Neuroma (Amputation ), suture granuloma Residual or reformed gallbladder Stump cholelithiasis |
| Liver | Chronic idiopathic jaundiceCirrhosisCyst Dubin-Johnson syndrome Fatty liver; hepatitis; cirrhosis; idiopathic jaundice Gilbert disease Hepatitis Hydrohepatosis Liver abscess Sclerosing cholangitis |
| Nerve | Intercostal lesionsIntercostal neuralgiaNeuroma Neurosis Psychic tension or anxiety Spinal nerve lesions Sympathetic imbalance |
| Pancreas | Benign tumorsFunctional pancreatic sphincter disorderPancreatic cysts Pancreatic stone Pancreatitis Stone Tumors |
| Periampullary | PapillomaSphincter of Oddi dysfunction (Functional biliary sphincter disorder); spasm; hypertrophyspasm; hypertrophySphincter of Oddi stricture Stricture |
| Small bowel | AdhesionsAdhesions; incisional hernia; irritable bowel diseaseIncisional hernia Irritable bowel disease |
| Stomach | Bile gastritisPeptic ulcer disease |
| Subcutaneous tissue | AbscessHematoma |
| Vascular | Coronary anginaInjury to hepatic artery, portal vein (pseudoaneurysm, portal vein thrombosis)Intestinal angina Mesenteric ischemia |
| Miscellaneous | Dropped GallstonesParasitic infestation (Ascariasis)Thermal injury Trocar site hernia |
| Other | AnxietyBacteria overgrowth in the stomachBarrett’s oesophagusBezoars Bile Acid Malabsorption Bile Reflux Bloating Celiac Disease Cramps Decrease in bile secretion Depression Diabetes Dumping of bile Syndrome Foreign bodies, including gallstones and surgical clips Gas Gastroparesis GERD Reflux Heartburn Irritable Bowel Syndrome Nausea Pain – right upper abdomen Pain – shoulders and abdomen Thyrotoxicosis Weight gain Weight loss |
Evidence based medical studies confirming statistically significant increased risk of cancer following cholecystectomy, required by law but never disclosed by doctors during the informed consent process listed as:
Anatomy |
Etiology |
| Other Biliary tract Liver Colon Esophagus Stomach Liver Liver Pancreas Periampullary Other |
Adrenal cancer Ampulla of Vater cancer Cholangiocarcinoma cancer Colorectal cancer (Colon / Bowl) Esophageal cancer Gastric cancer Hepatocellular carcinoma cancer Liver cancers Pancreatic cancer Periampullary cancer Smallintestine carcinoid cancer |
Source references:
- M. Farahmandfar, M. Chabok, M. Alade, A. Bouhelal and B. Patel, Post Cholecystectomy Diarrhoea—A Systematic Review, Surgical Science, Vol. 3 No. 6, 2012, pp. 332-338. http://dx.doi.org/10.4236/ss.2012.36065
- Tsai M-C, Chen C-H, Lee H-C, Lin H-C, Lee C-Z (2015) Increased Risk of Depressive Disorder following Cholecystectomy for Gallstones. PLoS ONE 10(6): e0129962. https://doi.org/10.1371/journal.pone.0129962
- Nudo R, Pasta V, Monti M, Vergine M, Picardi N. Correlation between post-cholecystectomy syndrome and biliary reflux gastritis. Endoscopic study. https://www.ncbi.nlm.nih.gov/pubmed/2699712
- Lorusso D1, Pezzolla F, Montesani C, Giorgio P, Caruso ML, Cavallini A, Guerra V, Misciagna G. Duodenogastric reflux and gastric histology after cholecystectomy with or without sphincteroplasty https://www.ncbi.nlm.nih.gov/pubmed/2253017
- Shah Gilani SN1, Bass GA1, Kharytaniuk N2, Downes MR3, Caffrey EF3, Tobbia I3, Walsh TN4. Gastroesophageal Mucosal Injury after Cholecystectomy: An Indication for Surveillance? https://doi.org/10.1016/j.jamcollsurg.2016.12.003
- Bistritz, L., & Bain, V. G. (2006). Sphincter of Oddi dysfunction: Managing the patient with chronic biliary pain. World Journal of Gastroenterology?: WJG, 12(24), 3793–3802. http://doi.org/10.3748/wjg.v12.i24.3793
- Donato F. Altomare, Maria T. Rotelli, Nicola Palasciano. Diet After Cholecystectomy http://www.eurekaselect.com/node/152535/article
- Wikipedia, Postcholecystectomy syndrome. https://en.wikipedia.org/wiki/Postcholecystectomy_syndrome
- Steen W Jensen, MD; Chief Editor: John Geibel, MD, DSc, MSc, AGAF Postcholecystectomy Syndrome [medscape.com]
- S.S.JaunooS MohandasL.M.Almond. Postcholecystectomy syndrome (PCS) [ScienceDirect]
- Sureka B, Mukund A. Review of imaging in post-laparoscopy cholecystectomy complications. Indian J Radiol Imaging 2017;27:470-81 [Indian Journal of Radiology and Imaging]
- Murshid KR. The postcholecystectomy syndrome: A review. Saudi J Gastroenterol [serial online] 1996 [cited 2018 Jan 15];2:124-37. Available from: http://www.saudijgastro.com/text.asp?1996/2/3/124/34017
- Girometti, R., Brondani, G., Cereser, L., Como, G., Del Pin, M., Bazzocchi, M., & Zuiani, C. (2010). Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. [The British Journal of Radiology, 83(988), 351–361]
- Jacob L. Turumin, Victor A. Shanturov, Helena E. Turumina. Irkutsk Institute of Surgery, Irkutsk Regional Hospital, Irkutsk 664079. The role of the gallbladder in human [ScienceDirect]
- Dr. Jacob L. Turumin, MD, PhD, DMSci Biliary Diseases Laparoscopic Cholecystectomy. Postcholecystectomy Syndrome. http://www.drturumin.com/en/index.html#sthash.Y35Uey8C.dpuf
- Martin, Walton. “RECENT CONTROVERSIAL QUESTIONS IN GALL-BLADDER SURGERY.” Annals of Surgery 79.3 (1924): 424–443. Print. [PMC]
- The NIDDK Gastroparesis Clinical Research Consortium (GpCRC). “Cholecystectomy and Clinical Presentations of Gastroparesis.” Digestive diseases and sciences 58.4 (2013): 1062–1073. [PMC]
- Yong Zhang , Hao Liu , Li Li , Min Ai , Zheng Gong, Yong He, Yunlong Dong, Shuanglan Xu, Jun Wang , Bo Jin, Jianping Liu, Zhaowei Teng Cholecystectomy can increase the risk of colorectal cancer: A meta-analysis of 10 cohort studies Published: August 3, 2017 https://doi.org/10.1371/journal.pone.0181852
- Mearin, F., De Ribot, X., Balboa, A. Duodenogastric bile reflux and gastrointestinal motility in pathogenesis of functional dyspepsia. Role of cholecystectomy. Digest Dis Sci (1995) 40: 1703. https://doi.org/10.1007/BF02212691
- Simona Manea, Georgeta & Carol, Stanciu. (2008). DUODENOGASTROESOPHAGEAL REFLUX AFTER CHOLECYSTECTOMY. Jurnalul de Chirurgie. 4 [Researchgate]
Another opinion not accepted by NZ Laparoscopic Surgeons or heath consumer watch dog Health and Disability Commissioner and as such never presented to patients when legally obtaining informed consent for gallbladder surgery (Cholecystectomy)
The body is permanently damaged and cannot be healthy without a gallbladder and its function. You can live, but in many cases you will be miserable. Some common side effects of gallbladder removal are an upset stomach, nausea, and vomiting. Gas, bloating, and diarrhoea. Persistent pain in the upper right abdomen.
It is gross medical negligence to send a patient home after surgery and pretend there are no side effects and can lead a perfectly normal life without a gallbladder and its purpose. Due to the considerable numbers of affected New Zealand patients, under United Nations Universal Declaration of Human Rights, Article 5 and 25 an ongoing crime is occurring.
Article 5: No one shall be subjected to cruel, inhuman or degrading treatment
Article 25: Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, or other lack of livelihood in circumstances beyond his control.
Most patients suffer permanent impairments of the digestive system as a consequence of cholecystectomy, and develop various disorders as a result of poor digestion. The gall bladder is a vital organ with a crucial role in the absorption of fat and fat-soluble vitamins A, D, E and K and in essential fatty acids (omega-3 and omega-6), and poor cholesterol metabolism. In the long run, this may contribute to fatty liver. The absence of the gall bladder affects not only the process of food digestion but a wide range of other internal processes as well. In time, patients who have suffered cholecystectomy are also exposed to a high risk of developing heart disease, diabetes and disorders of the nervous system. This is due to inappropriate synthesis and assimilation of vital nutrients, vitamins and minerals.
Vitamin deficiency |
Symptoms and Conditions |
| Vitamin A deficiency signs include | Dry eyes Drying, scaling, and follicular thickening of the skin Night blindness Red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks) Respiratory infections |
| Vitamin D deficiency linked to a strikingly diverse array of common chronic diseases, including: | Alzheimer’s disease Asthma Autism Cancer Cavities Cold and fly Crohn’s disease Cystic fibrosis Diabetes 1 and 2 Dementia Depression Eczema & Psoriasis Hearing loss Hypertension Heart disease Infertility Inflammatory Bowel Disease Insomnia Macular degeneration Migraines Multiple Sclerosis Muscle pain Obesity Osteoporosis Periodontal disease Preeclampsia Red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks) Rheumatoid arthritis Septicemia Seizures Schizophrenia Signs of aging Tuberculosis |
| Vitamin E deficiency signs include: | asthma and allergies brain damage cancer cognitive decline high oxidized LDL cholesterol levels hot flashes menstrual pain poor circulation prostate and breast cancers |
| Vitamin K deficiency can lead to: | Arterial calcification Cardiovascular disease Dementia Infectious diseases such as pneumonia Leukemia Liver cancer Lung cancer Osteoporosis Prostate cancer Tooth decay Varicose veins |
| Deficiencies in essential fatty acids | Allergies Alzheimer’s disease Asthma Bone weakness Brittle or soft nails Cancer Cracked skin on heals or fingertips Dandruff or dry hair Dry eyes Dry Eye Syndrome Dry, flaky skin, alligator skin, or “chicken skin” on backs of arms Fatigue Frequent urination or excessive thirst Gallstones Heart disease Lowered immunity, frequent infections Lupus erythematosus and other autoimmune diseases Multiple sclerosis Parkinson’s disease Peripheral artery disease Poor attention span, hyperactivity, or irritability Poor mood Poor wound healing Postpartum depression Premature birth Problems learning Red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks) Rheumatoid arthritis Schizophrenia Tissues and organ inflammation Ulcerative colitis Vascular complications from type 2 diabetes |
Source references:
- National Research Council. 1989. Diet and Health: Implications for Reducing Chronic Disease Risk. Washington, DC: The National Academies Press. https://doi.org/10.17226/1222. https://www.nap.edu/read/1222/chapter/14#317
- Mike Adams. What conventional medicine won’t dare tell you about gall bladder removal surgery. http://www.naturalnews.com/007733_gall_bladder_surgery.html
- Barbara Bolen, PhD. Emmy Ludwig, MD. What to Do About IBS After Gallbladder Removal. http://ibs.about.com/od/relatedconditions/a/IBS-After-Gallbladder-Removal.htm
Alternative opinions not accepted continued
The postcholecystectomy syndrome may occur in two weeks or two decades following gallbladder surgery. The symptoms can be mild and just diminish of person’s quality of life. For some patients, PCS makes life miserable. Mostly, it does not depend on upon the surgical techniques, equipment, or experience of the surgeon. Just absence of gallbladder causes this problem.
The typical symptoms of the postcholecystectomy syndrome include
- Intolerance of some foods, mostly fatty foods
- Upper abdominal pain
- Constant gas, bloating, flatulence
- Nausea, vomiting
- Stubborn heartburn
- Constipation
- Chronic diarrhea
- Symptoms, which are very far from stomach such as depression, anxiety, low memory, skin dryness or itchiness, yellowish skin, blurred vision, bruises, tingling and numbness, often colds and more
The problem is that there is no conventional treatment of the PCS. The patients are under the care of the variety of doctors and medical practitioners with different skills, knowledge, and viewpoint on the postcholecystectomy syndrome. There are three kinds of situations.
The first one is when the symptoms happen rarely, and the entire lab and visual tests are normal. Patient has symptomatic treatment with the painkillers or gets a referral to a pain management clinic, or sends to a psychiatrist for depression and anxiety. Frequently PCS misdiagnosed with gastroesophageal reflux disease, food poison or food sensitivity, gastritis, dyspepsia, IBS, dumping syndrome, etc.
The second situation, the lab, and visual tests demonstrate increases in the pancreatic or liver enzymes, presence of the dilatation of the common bile duct. Symptoms become chronic. That is followed by numerous diagnostic tests, which are often insecure, visits to the countless doctors, hospitals, and taking all sorts of medications.
The third scenario, the individual underwent many tests that revealed severe structural changes in the bile duct, pancreas, liver, duodenum, and sphincter of Oddi. At this time, patients have numerous doctor visits, medications, ER admissions, consultations of specialists, and endoscopic surgeries.
These three situations are not separate disorders; these are the different stages of the sphincter of Oddi dysfunction, chronic biliary pancreatitis, metabolic acidosis, dysbiosis, and adhesion syndrome. Biliary means connection to bile system. The health of the bile, bile ducts, sphincter of
Oddi, and gallbladder is inextricably bound to the health of the pancreas, small, large intestines, and stomach.
Like all chronic diseases, there are the functional stage, structural stage, and advanced stage of the postcholecystectomy syndrome
“In 12 years of practice, I have rarely met any ‘cholecystectomy patient’ who didn’t have to make changes to feel better afterwards. Sooner or later their underlying nutritional deficiencies caught up to them and affected their health.”
Dr. Miranda Jorgenson, licensed Chiropractic Physician